Abstract
Introduction
Ixazomib is an orally available proteasome inhibitor, shown to be safe and efficacious in combination with lenalidomide and dexamethasone (IRd regimen) in patients with relapsed and refractory multiple myeloma (RRMM) with 1-3 prior lines, demonstrating a progression free survival (PFS) benefit which was similar across cytogenetic risk groups (Tourmaline-MM1 phase 3 trial). A European real world data analysis of an IRd named patient program (NPP) outcomes in Greece (n=35), UK (n=46) and Check republic (n=57) showed similar favorable outcomes (Terpos et al, Blood 2017 130:3087). We aimed to analyze outcomes of ixazomib combinations among a multi-site cohort in the Israeli Myeloma registry. Overall response rate (ORR) was classified according to IMWG criteria. Primary endpoint was PFS, secondary endpoints included ORR, overall survival (OS), safety and tolerability.
Patients
A total of 78 patients across 7 sites, who received at least one cycle of ixazomib combination between June 2013 and June 2018 for treatment of RRMM were retrospectively included. Median age was 68 (range: 38-90). Male/Female ratio was 42/36. ISS (rISS) I/II/II was 30%/42%/27% (25%/54%/15%). Patient received between 1 and 7 prior lines of therapy, 66% received ixazomib in 2nd line, 18% in 3rd line. Overall, 89% of patients had been exposed to PIs (bortezomib 86%) prior to IRd, 41% to IMiDs (thalidomide 28% lenalidomide 22% and pomalidomide 6%), and 35% had undergone autologous transplantation (ASCT). Induction treatment was mostly bortezomib based (85%), most frequently VCD (62%). FISH cytogenetics were available for 60 patients, 29 (48%) had high or intermediate risk aberrations (t(4:14) 12 pts, amp 1q21 12 pts, del17p 9 pts). Disease aggressiveness was classified by treating physician as indolent (rapid control to protect from target organ damage not required) vs aggressive (imminent target organ damage) in 63% vs 27%, respectively. 60 (77%) of the 78 patients received ixazomib via a named patient program, the rest via national or private healthcare provider.
Results
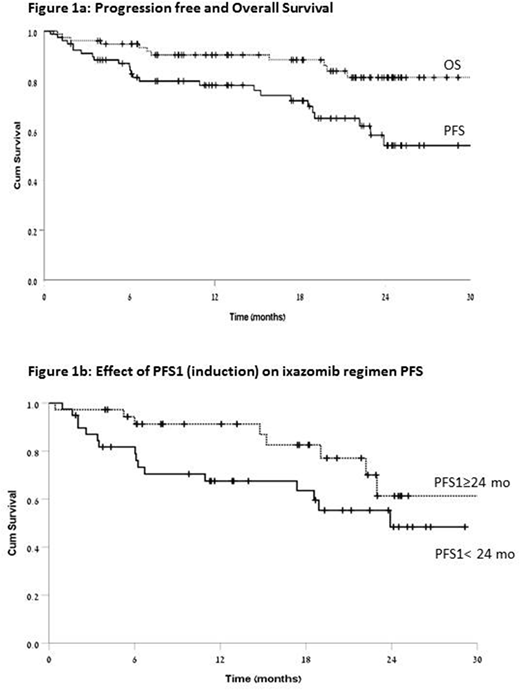
Median time of follow up from first ixazomib dose was 22 months (range: 1-39 months), and 54 months from diagnosis of myeloma. Treatment is ongoing in 44 (56%) patients with a median duration of 19 months (range: 1-29). Among patients who discontinued treatment, the median duration was 9 months (1-31). Ixazomib was combined with lenalidomide, pomalidomide, and daratumumab in 69%, 9% and 4%, respectively. Overall response rate was 88% - CR 10%, VGPR 36%, PR 42%. Progression free survival was 78% and 54% at 12 and 24 months, respectively (fig1a). A worse PFS was found with physician assessment of aggressive vs indolent disease (14.5 vs 25.9 months, p=0.001), and with post induction progression free period (PFS1) ≤ 24 months vs. >24 months (23.9 vs 31.5 months, p=0.038) (fig 1b); age >=65 trended towards a worse PFS (p=0.058). Poor cytogenetic risk, prior exposure to bortezomib, prior auto transplant, and number of prior lines of therapy did not affect PFS or ORR. OS from first ixazomib administration was 90% and 81% at 12 and 24 months, respectively; median OS was not reached (fig1a).
Any (grade 3-4) toxicity considered by investigator as related to ixazomib was reported in 70% (18% grade 3-4), including neutropenia 14% (6%), anemia 19% (6%), thrombocytopenia 17% (5%), nausea and vomiting 17% (1%), DVT/PE 4% (1%), neutropenic infection 0 (4%), peripheral neuropathy 14% (3%), diarrhea 14% (3%), rash 10% (4%), pneumonia 5% (3%). There were no ixazomib related deaths. Dose reduction or discontinuation due to toxicity occurred in 28% and 12%, respectively.
Conclusion
Our data shows ixazomib-based combinations are efficacious and safe regimens for patients with RRMM, achieving ORR of 88%, at 2nd as well as later lines of therapy, regardless to cytogenetic risk. Over a median follow up of almost 2-years, 54% remained progression free at 24 months. An ixazomib based regimen may be particularly attractive for patients who remain progression free for more than 24 months after a bortezomib induction and for patients with a more indolent disease phenotype.
Cohen:Neopharm Israel: Consultancy, Honoraria; Takeda: Consultancy, Honoraria, Research Funding; Amgen: Consultancy, Honoraria, Research Funding; Janssen: Honoraria, Research Funding; Medisson Israel: Consultancy, Honoraria, Research Funding. Tadmor:NOVARTIS: Consultancy; PFIEZER: Consultancy; ABBVIE: Consultancy; JNJ: Consultancy; ROCHE: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal